- Home
- Wat is stress?
- PTSS uitleg
- PTSD explained
What is PTSD (Post Traumatic Stress Disorder) ?
Ga HIER naar de Nederlandse versie van deze pagina
First of all, the definition from the DSM-5, the psychiatric manual.
PTSD (post-traumatic stress disorder) has the following official criteria:
A. Exposure to actual or threatened death, serious injury, or sexual violence in one or more of the following ways:
- experiencing the traumatic event yourself
- personally witnessed (seen, read or heard) this traumatic event that happened to others
- hearing, reading, seeing that the event happened to a close family member or close friend. The event must be violent in nature or involve an accident.
- experiencing repeated or extreme exposure to the horrific details of the psychotraumatic event. (This does not apply to exposure via digital media, film, TV or photographs, unless work-related).
B. One or more of the following intrusive symptoms must be present; those symptoms must be related to the traumatic event and have started after that event has occurred.
- Repetitive, involuntary and intrusive painful memories of the traumatic event
- Repetitive bad dreams in which the content and/or feeling (affect) of the dream is related to the traumatic event
- Dissociative reactions (such as flashbacks) in which the person feels or even acts as if the traumatic event is happening again. In an extreme form, the person may have lost sense of reality (= dissociation).
- Intense or prolonged psychological distress upon exposure to internal or external stimuli that symbolize or resemble an aspect of the traumatic event
- Marked physiological (physical) responses to internal or external stimuli that symbolize or resemble some aspect of the traumatic event
C. Continued avoidance of stimuli associated with the traumatic event. This avoidance started after the traumatic event and is evident from one or both of the following characteristics:
- avoidance or attempts to avoid painful memories, thoughts, or feelings about, or strongly associated with, the traumatic event
- avoidance or attempts to avoid external aspects that are reminiscent of the traumatic event (e.g. people, places, conversations, activities, objects), or that evoke painful memories, thoughts, feelings strongly associated with the traumatic event.
D. Negative changes in cognitions (thoughts) and mood associated with the traumatic event and starting after the event, as evidenced by 2 or more of the following:
- Inability to remember an important aspect of the traumatic event (usually due to dissociative amnesia, not due to neurological injury or drug use)
- Persistent and exaggerated negative ideas or expectations about oneself, others, or the world (e.g., “I am bad,” “no one can be trusted”)
- Persistent, distorted (abnormal) cognitions about the cause or consequences of the traumatic event such that the person blames himself or others for it (to an extreme degree).
- Persistent negative mood (e.g. fear, anger, guilt or shame)
- Markedly reduced interest in or participation in (previously) important activities
- Feelings of detachment or alienation from others (no longer feeling connected)
- Constant inability to experience positive emotions (e.g. happiness, satisfaction, or loving feelings)
E. Marked changes in arousal and reactivity associated with the traumatic event. These started or worsened after the traumatic event, as evidenced by 2 or more of the following:
- Irritable behavior and outbursts of anger (with little or no provocation, sudden), usually manifested by verbal or physical aggression against people or objects
- Reckless or self-destructive behavior (e.g. speeding, drug use)
- Hypervigilance (being overly vigilant)
- Exaggerated startle responses
- Concentration problems
- Sleep disturbance (difficulty falling or staying asleep, restless sleep)
F. The duration of the above is longer than 1 month
G. The disorder must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
H. The disorder is not caused by the effects of a substance (e.g. medication or alcohol or other drugs), or by a physical condition
Furthermore, PTSD is also possible with:
- Dissociative symptoms:
- depersonalization: feelings of alienation from one's own psychological processes or body, as if the person is experiencing himself from outside, e.g. seem to be in a dream, or that the body feels unreal, or that time passes very differently
- derealization: as if the reality around the person is not real, as if in a dream or balloon, as if environment is strange or distorted
2. The PTSD can also be with delayed expression: where all criteria are only met after 6 months and not completely before that.
Notable key points of PTSD
So you have to meet quite a few criteria if you want to officially speak of Post Traumatic Stress Disorder. In clinical practice, this does not always appear to be the case, so clinicians often do not diagnose PTSD. That is a shame and bad because the person himself does indeed have serious complaints and therefore gets stuck or is in danger of getting stuck in daily life.
Another diagnosis that can often be made is Other (un)specified trauma and stressor-related disorder. The main criterion A (having experienced a trauma) is met, but not all mandatory criteria of B, C, D and E are met, while there is significant (disruptive) suffering for someone.
Yet another frequently diagnosed diagnosis is acute stress disorder. In fact the same as PTSD, but the symptoms last longer than 1 day but also less than 1 month.
The CORE points of a PTSD or trauma-related disorder are in fact clear:
- an event must have been intensely emotional for the person, causing his/her feelings and ideas to change fundamentally, in a negative sense.
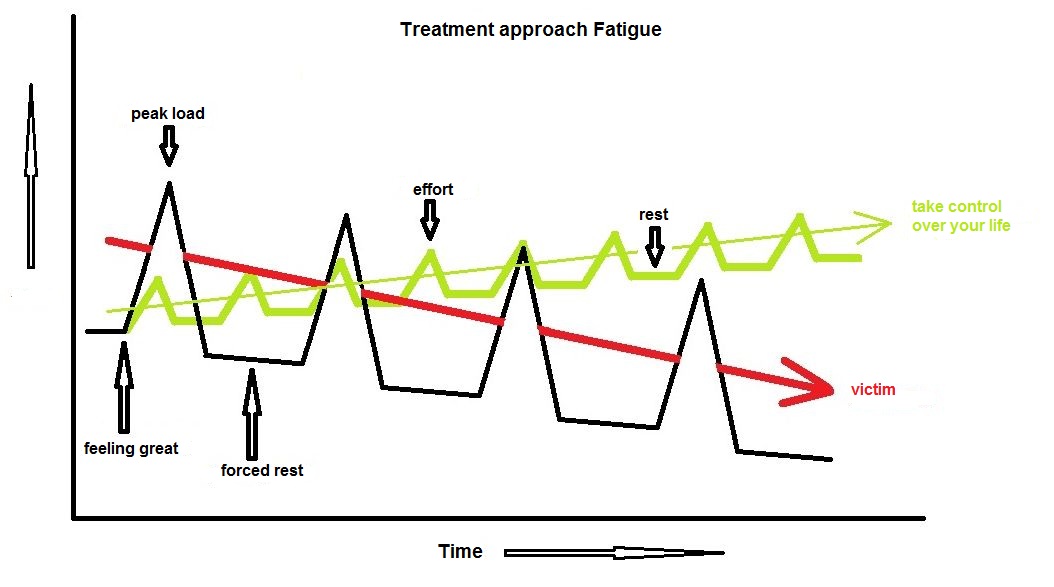
- Someone's thoughts and feelings no longer return to a manageable form: someone continues to feel a significant negative impact after 1 month. E.g. due to poor sleep, being constantly stressed and not being themselves. The stress response system remains 'on' and does not relax.
- The traumatic event and all its aspects continue to haunt the person's head and body and the person is therefore constantly triggered. Anything similar can trigger/evoke this event, so that the person has the feeling of reliving the event over and over again with all the stress/emotions related to it.
- Not everything about the traumatic event can be remembered by the client. Often only a few (very unpleasant) images, sounds or smells of such a traumatic event are remembered. However, it is also possible that this memory is not entirely truthful. Often the memory is distorted and (nasty) things can be made up by our consciousness.
How often does PTSD occur ?
This is an essential question, but difficult to answer. In scientific studies, estimates of the prevalence of PTSD vary considerably, from 1.1% to as much as 6.8% (see 2017 article here).
Another German article from 2020 mainly shows the economic impact of PTSD by using data from Germany. They also estimate the prevalence, but the estimate is from 2010 and it is emphasized that the prevalence of PTSD (occurrence) is low (1.1-2.9%).
In general, studies assume (estimate) that the prevalence is higher in women than in men: on average, women develop PTSD more often than men. Why is never made clear or unknown.
As is well known in the scientific world, there are many studies. These studies often cross-reference each other and are often cautious with their estimates. Gambling is not something scientific. But...my clinical impression and that of my colleagues is that PTSD and other trauma- and stressor-related disorders are indeed much more common than scientific estimates. Possibly between 10-15% of the population. But in all honesty: no one can state this precisely, because no one has kept track of it exactly. Due to strict privacy rules, it is also not possible to get a good idea of how often PTSD actually occurs.
Because of what or why does PTSD develop ?
Another very important question and unfortunately...no one knows it exactly. The more you read about it, the more interesting it becomes, but - as is often the case - the more questions remain unanswered.
The fact is that PTSD can only arise when there is a threat, i.e. when there is danger. Even more specific: with EXPERIENCED danger. Even if there is no danger, but someone thinks he/she is in serious danger, PTSD can develop. This fact is essential in understanding how our nervous system, especially our brain, reacts and can cause PTSD.
There is another very interesting fact: the majority of people who are confronted with a traumatic threat (nasty event) does not develop PTSD. However, there is often an acute stress disorder immediately after such an event, certainly a few hours or days afterwards. In fact, this can also be considered completely normal. But only between 1.6 to 7% of people actually get PTSD from this. However, it is possible that more people continue to suffer from it for longer than 1 month, but that their symptoms are not severe enough for a PTSD diagnosis. Then it is often another (un)specified trauma and stressor-related disorder. I suspect that this diagnosis is much more common, possibly up to 20% of people. But virtually no scientific studies have been conducted on this.
I would like to discuss the suspected neuropsychological mechanism that causes a PTSD or trauma-related disorder below. It is largely composed of my neuropsychological knowledge of emotions, cognitive functions and our behavior (which is of course limited), my clinical experience with treating people with trauma (hundreds) and the stories of colleagues, speakers at symposia and those from books, about traumas.
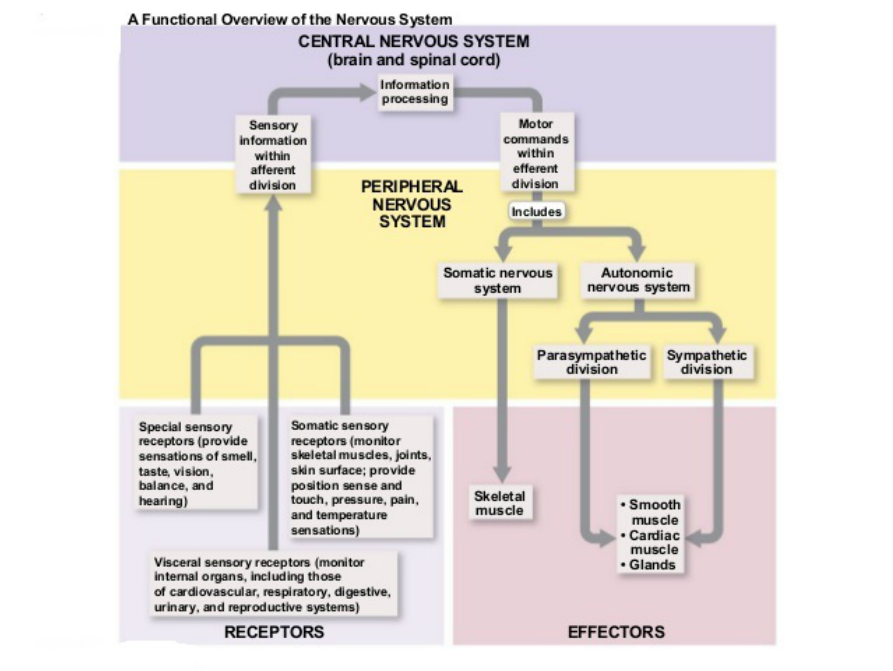
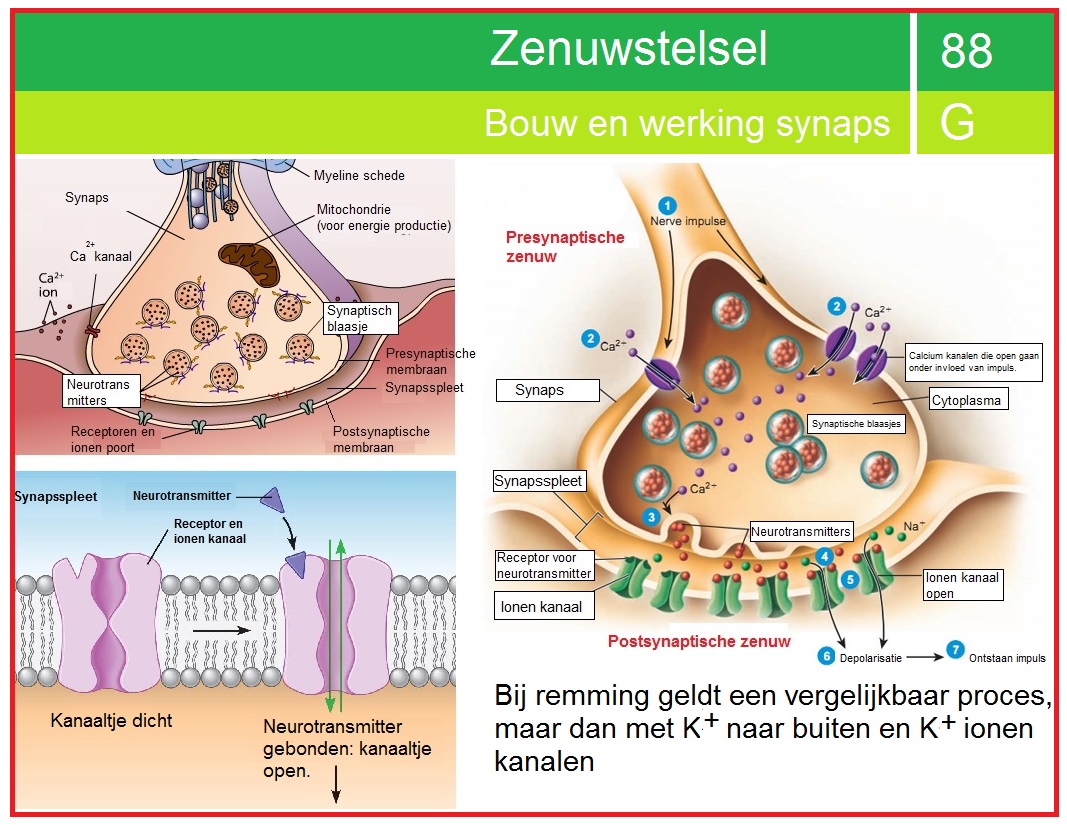
A threat or danger leads to a strong reaction in our nervous system, especially our autonomic nervous system = the stress response. This autonomic nervous system has 2 main branches: the parasympathetic and the sympathetic part. The parasympathetic part is the part that ensures peace, calmness and a strong decrease in heart rate. The 10th cranial nerve, the vagus nerve, has the most branches within this autonomic nervous system to almost the entire body.
The Sympathetic part of the autonomic nervous system is responsible for activity and getting into action when danger occurs. The extreme form of this is the flight-or-fight response. If this mobilization of the body does not allow you to escape the danger, the freeze reaction (stiffening) may occur: the body coming to a complete standstill, in the hope that you will no longer be seen and can thus be saved (or escape) from your attacker.
This is clearly visible in the animal world, e.g. sheep, goats or chickens. It looks funny, but it is a serious evolutionarily developed reflex that occurs autonomously in extreme fear of death. It is the last possibility to escape your death. In a beautiful YouTube video, an Impala antelope escapes death by applying this reflex. Click on the image below to view the YouTube video.
The above video is especially so interesting because it shows something else essential about psychotrauma. The body initially responds with the autonomic stress response, which is the most extreme: dissociating, actually consciousness 'leaving' the body, pretending to be completely dead. This is the dorsovagal response of the vagus nerve that reduces many bodily functions such as heart rate, breathing, blood pressure and muscle tension very quickly and significantly. Consciousness is almost certainly also reduced. In other words: the memory storage process will no longer function completely in this state: not everything will now be remembered or stored (hence dissociative amnesia).
Secondly, once the danger has passed, the near-dead body must become active again. The video clearly shows that the Impala starts breathing heavily (particularly belly breathing) and the ear also moves briefly. With such heavy breathing, much more oxygen is taken in and the heart rate goes up, including higher blood pressure and muscle tension. This is accompanied by severe shaking and jerking, probably partly caused by the effects of some stress hormones such as adrenaline (heart rate increasing) and cortisol. Eventually the body gets going enough and the shock subsides. The Impala then gets up remarkably quickly and flees from the dangerous spot.
In particular, Peter Levine, the trauma expert and author of the book The Tiger Awakens (see recommended books), also talks about the necessity of fully completing all trauma-related body movements. He suspects that PTSD is partly due to the freezing and abrupt termination of the entire processing process that is part of a trauma experience. That is why, in his treatment of psychotrauma, he often stimulates clients to make movements that he suspects could NOT have been completed at the time of the trauma.
It is striking that afterwards the trauma is often no longer present in the body, it is no longer 'frozen', as it were. It seems that the entire memory trace associated with trauma processing finally fades away in long-term memory. I realize this sounds a bit speculative, but I do not see another way to make it more clear. I will explain it a little further later: my suspicions about how things work with PTSD. The animal world is essential here because our brains are built on an animal brain.
Psychotrauma and memory
It is still not entirely clear why psychotrauma takes root in the brain of one person and not in many others. I try to explain my ideas about this below.
First of all, the well-known fact is that an event is stored by the brain in the short-term memory, or rather: in working memory. That is the highly volatile memory that only exists for a few seconds (up to about 15-20 seconds). Within the limited space of that working memory (one thinks about 5-8 units of information at the same time, different per person), all kinds of details of an event are processed.
During an unpleasant event with a threat, the intense (basic) emotion of Fear automatically lets someone focus on the most dangerous details of the event. For example, during a rape where the rapist stands in front of you with a knife, your consciousness (= working memory) may be filled with the eyes of the rapist or the knife itself. That just depends on how strong these stimuli are clearly visible. Another example is the bad stinking mouth of the rapist that can be stored extremely well. The fact is that such details, accompanied by severe anxiety, are best stored in your long-term memory.
The route from working memory to long-term memory does not happen overnight. Actual consolidation (= reliable and efficient storage in the Long-Term Memory) appears to take several hours and sometimes several days. This often requires a good night's sleep. That night's rest is necessary for the memory storage processes to run optimally.
This is probably one of the causes of developing PTSD. A good night's sleep is usually NOT the case after a psychotrauma: restless sleep or even no sleep at all. This probably means that some very unpleasant elements/details of the event are constantly repeated in working memory, with the necessary strong emotions. From memory theories we know that such unpleasant details are stored extremely well in Long-Term Memory. It is possible that such details are 'burned in', as it were, and deep memory traces are formed in Long-Term Memory. All kinds of other details of the event may also be stored, but not very reliably.
What many people do not know is that not only all kinds of details of an event are stored, but also details of the immediate environment, such as colors, sounds and smells. And even more importantly: the internal body state is also stored at the same time. So e.g. your blood pressure, your breathing, your muscle tension, your posture, the amount of (stress) hormones in your blood, your heart rate.
The so-called memory image of an event is therefore extremely complex and also very layered. After all, your body condition is stored via other brain areas than, for example, the details of the immediate environment. Many brain areas that are active at that moment are involved in storage in Long-Term Memory.
This important detail, that a memory image of an event consists of a layered representation of the event itself, your body condition, and parts of the immediate environment, can explain why, for example, a certain body position can immediately trigger intense fear or sadness after a traumatic event. Many people say that the trauma is stored in the body, but in fact that is NOT entirely true. The only thing that can be said is that the traumatic event together with parts of the body condition is stored in Long-Term Memory (in the brain). This storage process after a trauma in Long-Term Memory is depicted below.

Process of Storage in Long-Term Memory after Psychotrauma
Above is the Storage process that takes place after a traumatic event. It hopefully becomes clear that the Memory Image consists of several details such as the Internal and External environment and also parts of the event itself. Strong emotions such as Fear (or Anger or Sadness) have a strong influence on how something is stored in Long Term Memory.
We know that intense emotions, together with unpleasant details, are strongly stored in Long-Term Memory. Long-Term Memory is in fact a very large associative network: everything is linked together. The links are particularly strengthened by emotions. If the basic emotion is fear, all events in your life that involved fear are linked together. This may explain why in a panic attack (= severe fear) you can remember all kinds of very fearful images and events more quickly than normal, neutral events.
In memory theory this is also called 'State-dependent learning'. A clear example of this is if you learn something when you are drunk, i.e. under the influence of alcohol. Learning then takes place, certain things are stored in your head, but at the same time your body condition is also stored, under the influence of alcohol.
Click on the image below to see a YouTube video explaining the different forms of memory and context/state-dependent learning.
Video clip about Context-dependent learning
It is a nice and simple explanation about context (or state) dependent learning and memory.
Why does the memory of a traumatic event NOT disappear in PTSD ?
Although I have described above how a traumatic event most likely is stored in Long-Term Memory, I have not yet explained why it also remains there in PTSD. Because from a neuropsychological perspective, an unpleasant event is stored in LTM (Long-Term Memory) in exactly the same way as other, more neutral events.
To understand all this you have to look at the difference between a traumatic and a neutral or positive event. In my opinion, that difference boils down to 2 essential things:
- The Intensity of an unpleasant emotion (Sadness or Fear). A very large, sudden change in one or more core beliefs that seriously damages the self-image.
- Both factors MUST occur or PTSD will not develop. So just 1, a strong emotion, is not enough for PTSD to arise.
After all, in the event of a positive event, such as e.g. a very intense crush, or laughing terribly hard with friends, or fun dancing to great music, although a very intense emotion such as Happiness is present, the major change in a core belief and thus the damage to the Self-image is missing.
I think this damage to self-image is essential and necessary to develop PTSD. I based this on all my clients (and there are now hundreds) that I have treated for PTSD or other trauma and stressor-related disorders. All of these clients had suffered a serious, very sudden change in their Self-image after the traumatic event. And this change was so great that their self-image was seriously weakened. This applied in most cases to both dimensions in the Self-image: both in Self-control and in Self-esteem. It was also striking that these clients with PTSD did not realize that their Self-Image was so damaged and therefore they could no longer repair it themselves. They lacked sufficient self-control for this.
The essential element capable of causing such very rapid and large changes in a Self-image is an Intense emotion, generally Fear. That can only happen if someone experiences a danger. And that has everything to do with a Self-image that is not very strong, or in other words: not realistic. That intense fear seems to trigger a normal stress response in which the sympathetic nervous system comes into action: flight or fight.
And precisely when there is insufficient self-control, the autonomic nervous system can switch the stress response to a very extreme reaction: a psychological shock. Then someone dissociates (consciousness is greatly narrowed), all actions are, as it were, frozen and are no longer helpful, movement hardly occurs anymore, angry emotion disappears and fear takes over completely.
After all this, self-image has changed significantly and rapidly, with both self-control and self-esteem severely reduced. The old Self-image (Self) is completely different from the new, damaged Self. That is also one of the clearest characteristics of PTSD: one no longer recognizes oneself, is very different than before: more anxious, more jumpy, no longer enjoys oneself or things as much, often angrier, more easily irritated, much more feelings of guilt and lower self-esteem. In the figure below I have summarized the essential changes that lead to PTSD.
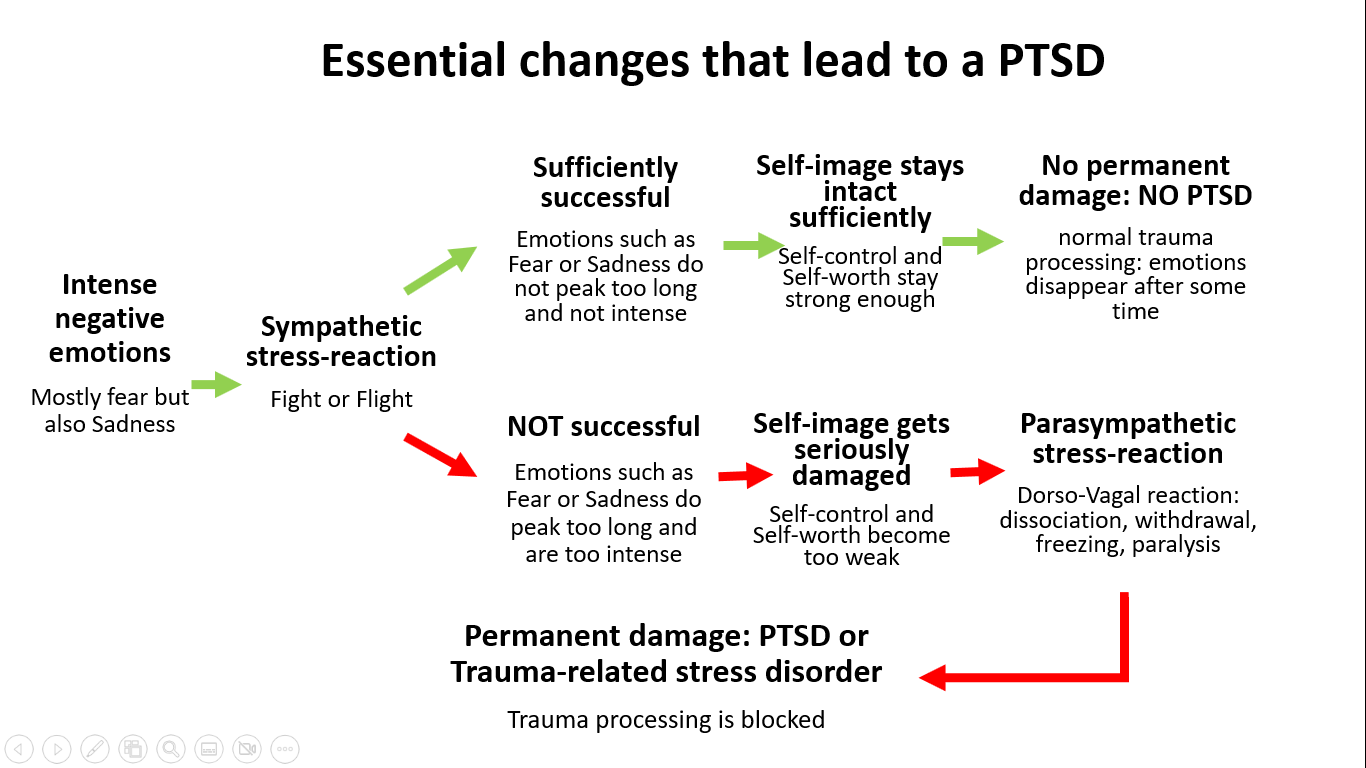
Essential changes that lead to PTSD
During a traumatic event, intense emotions arise that provoke a sympathetic stress response. This is intended to defend yourself and reduce the danger. However, if this is not successful, the stress response becomes a dorso-vagal reflex that can lead to abnormal (non)processing of the trauma. An essential element in this process is the Self-image, which plays a key role in whether or not PTSD develops.
Self-image is the key to the development and treatment of PTSD
As shown in the figure above, in my opinion the Self-Image is the key to explaining the development of PTSD. This model makes several predictions that I have been able to test based on my experiences with many clients with PTSD and with the EMDR treatment for these people. Unintentionally, they helped me a lot in understanding the PTSD condition.
The model predicts several things that I would like to explain per case below.
- With a sufficiently strong self-image, PTSD will not arise.
Explanation: every person (and animal) will show the sympathetic stress response to a threat because that is how our brains have evolved in that manner. This stress response is a defensive response that should reduce the (threatening) danger. However, for this response to be successful, you must have a sufficiently strong self-image. For more detailed information about this self-image, see my page about the Self-Image Model: click HERE for this page.
Your Self-image has 2 fundamental dimensions: Self-control and Self-esteem. Both must be strong enough to withstand any stress. The basic emotion of fear that arises from a threat can be regulated, i.e. reduced, if your self-control is strong enough. Self-control is the fundamental belief about yourself that you have the power to positively change things around you and within yourself. In psychology this is called the Internal Locus of Control. There are many studies about Locus of Control and many show quite a strong relationship with Internal locus of control and lesser psychopathology, supporting my hypothesis that a strong Self-control is a strong defence against emotional disorders such as PTSD. Just Google for studies on Internal locus of control. Here you can find a recent Spanish study (2023).
For example, the idea and confidence that you are strong enough to deter or even injure an attacker. But also e.g. the idea that you have the power to run away or to scream for help. Or the idea that you are able to talk to your attacker so that he or she becomes less aggressive.
In addition, your self-esteem is also important in the event of an impending danger. You must fundamentally believe in your self-worth: that YOU deserve to be there, that YOU are worthwhile and have certain rights. That no one may take away these rights. After all, if you really think that you are nothing, that you are just a good-for-nothing, then your defensive reaction will be much less strong. You will be much more likely to drop your head and wanting to withdraw and do nothing. Your coping style will likely be much more passive than what is needed to resist the threat.
2. If expectations are realistic, PTSD will not develop.
A sufficiently strong self-image is also a more realistic self-image. Your expectations and ideas about people and the world around you are realistic. You are rarely faced with surprises. That is why you will be much less shocked or completely upset if you experience something very severe. The emotions will usually be less intense because the difference between your expectations and reality is not large. That is also one of the reasons that care givers, who are emotionally attuned to very unpleasant situations, do not easily develop PTSD after just one event. Here too it is about the right mix between internal and external Locus of Control. If you know very well about what you really have (internal) control over and about what you do not have any control over because this is often beyond your reach, then you have an optimal balance between internal and external locus of control.
A good website that explains more about the right balance can be found HERE.
3. It is NOT about the seriousness of the threat but about the EXPERIENCED threat.
The DSM-5 is based on threats that are recognizable to everyone, such as rape, hostage taking, traffic accidents or assault. But there are also other psychotraumas that can lead to PTSD or a trauma-related disorder. This often is the case when someone's integrity, both physically and emotionally, has been seriously damaged.
An example: I once had an older lady (75) who had suddenly lost her dog (which she had had for 12 years) due to cardiac arrest. She found him dead in the kitchen with vomit next to him and he had also let go of his urine. The death had apparently been quite intense for the animal. After that she was completely upset. For weeks afterwards she could not fall asleep peacefully, she hardly ate anymore (no appetite) and also had bad dreams in which she or others around her died or had an accident. Remarkably, she did not dream about her deceased dog, but during the day she regularly had the image of her dog lying there helplessly in her kitchen. Almost every time she went into this kitchen, that image would involuntarily come back to her and she would become upset again.
In her case, the GP did not think of PTSD but of normal grief. He had not asked about the symptoms of PTSD. He wanted to prescribe her an anti-depressant. But that doesn't sufficiently treat her PTSD. How is it possible that she got stuck dealing with the death of her dog?
The model predicts that her Self-image would not have been strong enough. Moreover, the trauma also deeply affected her self-image. How? To her, her dog was no ordinary dog. Five years ago, she had lost her husband to cardiac arrest after 50 years of marriage. She and her husband often took long walks with their dog. Both were absolutely crazy about their dog. She felt useful as a person to take care of her dog. Her life mainly had meaning because she had her dog, especially after her husband died. She had promised him at the funeral that she would take care of their dog forever. And now that was no longer possible. Now her life had little meaning anymore. Moreover, she had felt guilty because she had not noticed in time that her dog had been in pain during the night (she thought so because she had seen the vomit and the pee).
These apparently small details are essential for her self-image. These details can therefore explain why her self-image was so seriously damaged by the death of her dog that she did not undergo normal grieving. She had developed the lighter form of PTSD (another trauma- and stressor related disorder). Every care provider who had made an effort to get to know her better had seen how such a trauma could damage her self-image very deeply and could therefore explain why she developed a trauma related disorder. That is why the nature of a trauma or threat is not very important, no matter what a psychiatric manual says about it.
I once read another wonderful example on the Internet from a child psychiatrist. A small 4-year-old child had developed a strong fear of peeing or pooping in the toilet at home. The parents had no idea why that had happened. The child slept poorly and was constantly afraid to go to the toilet at home, but this also appeared to extend to other toilets elsewhere. These fears also caused the child to become constipated.
The psychiatrist thought he would take a look at that toilet at home, but there didn't seem to be anything wrong with it. Not dirty, a normal toilet. The flush button was also easily accessible for the child and the light functioned normally. Until the psychiatrist flushed the toilet a few times. Only then did he notice that the toilet made a somewhat 'grunting' sound when flushing, but that was not the case with every flush. When the child who was in the living room with his parents heard the flushing, he completely froze and crawled away towards his mother. The psychiatrist thus discovered that it was that sound that the child was so afraid of. So it seemed like a specific phobia of a scary sound, rather than PTSD or trauma-related stress disorder.
However, he decided to have an extensive conversation with the 4-year-old child. About what events had taken place during the time these complaints started. Ultimately, through these conversations with the child and his parents, he discovered that this child really liked Disney movies. But at the age of 4, he watched a Disney movie with his dad that involved lions. And one lion in particular had frightened him very much, when this lion had roared intensely.
The mother could still remember that around that time her son suddenly had trouble sleeping and often had nightmares of being chased by animals (and lions). They had not yet told the psychiatrist that until he asked about what their son did and did not like. However, the psychiatrist had made the link between the sound of the toilet and this psychotrauma from that lion film. In fact, the psychotrauma was not the toilet but the scene of the roaring lion and the fight afterwards in the film. That had made a deep impression on the child.
His self-image was damaged here because he thought he was in danger at home. Especially when that nasty sound in the toilet sounded so much like that lion. The Powerless Demon had also become stronger in this child: of course he did not know what he could do against this Danger. And it kept happening every time he went to the toilet. Ultimately, the problem was solved by drawing therapy and by changing the sink so that flushing made a completely different, friendlier sound. Sometimes, it can be that simple.
Can you measure and strengthen your Self-image ?
To both questions I can wholeheartedly say: YES!
Many people know too little about their self-image and that is not surprising because it is an unconscious dynamic construct and process. It sits in your Long Term Memory and only through special questionnaires and special questions and self-reflection (= looking at yourself) will you get to know this unconscious Self-image better and better.
My page about the Self-Image Model provides much more explanation about the Self-Image. In addition, you can also actually measure your Self-image with the help of some personality questionnaires (PBQ126 and YSQ3). This measurement of the Self-image has been developed by me, so it is experimental, i.e. not yet scientifically investigated, but... it is useful.
I suggest that you delve more into your Self-Image and complete the aforementioned questionnaires PBQ126 and YSQ3. You will find your Self-Image Strength in the report that is automatically sent to you. It is a number between 0 and 100%. The average of this strength from both questionnaires is the best estimate of your Self-Image Strength. In healthy people who have few emotional problems, a healthy self-image should be between 75% and 100%. Read this page about the Self-Image Model and complete the questionnaires on this page. Have fun!
Have A Great Story About This Topic?
Do you have a great story, remarks or any additions to or about this? One that could help other people as well and above all is constructive? Then please share it!
DISCLAIMER
I will not take any responsibility for how the information on this website will affect you. It always remains your responsibility to handle all information with care and in case of medical or mental problems you should ALWAYS consult a professional in your neighbourhood!
Ik neem geen enkele verantwoordelijkheid voor hoe de informatie op deze site u zal beïnvloeden. Het blijft altijd uw verantwoordelijkheid om al deze informatie zorgvuldig te bekijken. In het geval van lichamelijke en/of mentale problemen dient u ALTIJD een professional in uw directe omgeving te waarschuwen!